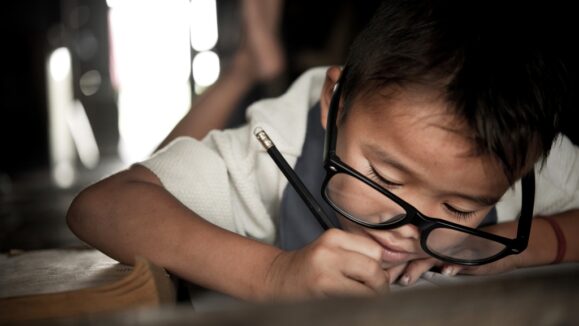
Myopia is on the rise worldwide, with the International Myopia Institute estimating that nearly half of the world will be myopic by 2050.1 Optometrists and ophthalmologists play crucial roles in the management and treatment of myopia, and their collaboration is essential for optimizing patient outcomes.
In recent years, myopia has reached epidemic proportions in many parts of the world, particularly in East Asia. However, studies1 indicate that myopia is also increasing at an alarming rate in other regions, including North America, Europe, and Australia. This global trend has prompted a shift in the approach to myopia management, focusing on proactive interventions to slow down its progression and reduce associated risks.
“I’m very concerned with myopia because it is definitely progressing. We have a lot of evidence of that,” said Dr. Elise Kramer, a residency- trained optometrist in Miami and an expert in specialty contact lens design and fitting.
“Fifty percent of Asian children are myopic, and we are going to reach that 50% here eventually if we don’t slow it down. So, I’m a huge proponent of myopia management and control. It is very relevant not just in my practice, but all over the world,” she continued.
Enhancing co- management practices for improved patient outcomes
Traditionally, optometrists have been primarily responsible for prescribing corrective lenses to improve visual acuity, while ophthalmologists have focused on surgical interventions and the management of ocular diseases. However, the management of myopia requires a comprehensive and collaborative approach involving both specialties.
“Unfortunately, although the rise in myopia rates has been well- documented in scientific literature, many practitioners are not fully aware of the extent of the problem and have little time to focus on it. Addressing these knowledge and time gaps is essential for promoting the adoption of effective myopia management strategies,” Dr. Kramer said.
“A lot of practitioners are overloaded with patients. Some work in big corporate enterprises and they get scheduled for six patients an hour,” she added. “A second reason is lack of resources or availability of equipment or products.”
Prof. James Wolffsohn, a UK-based professor of optometry and co-author of a recently published study2 on myopia management, agrees that practitioners need more resources, in addition to time, when it comes to myopia management.
“It is less of a knowledge gap (and more about) making products available to them and encouraging them to engage,” he said.
Ophthalmologists may have resources optometrists don’t, and vice versa.
“It’s a very good collaboration because obviously surgery is out of the scope of my practice,” Dr. Kramer said. “Open communication about what we’re doing for this patient and how we’re managing the case together is essential to have.”
“Eye care professionals working together always benefit patients due to more joined-up care,” noted Prof. Wolffsohn.
Beyond traditional single-vision interventions
Despite the increasing awareness of myopia as a public health concern, many practitioners still primarily prescribe single-vision interventions, such as glasses and contact lenses, without implementing additional strategies.
“Single-vision spectacles and contact lenses are well established for correcting myopia (allowing children to see clearly) and are very safe, but research shows they do not slow progression,” Prof. Wolffsohn explained.
Several strategies have been shown to effectively slow down the progression of myopia and reduce associated risks. These include orthokeratology (corneal reshaping contact lenses), multifocal contact lenses, atropine eye drops, and behavioral modifications such as increased outdoor time and reduced near-work activities. Optometrists and ophthalmologists need to be knowledgeable about these strategies and consider their incorporation into their clinical practice.
“Many myopia control approaches have been shown in robust clinical trials to slow the progression of myopia (compared to wearing a traditional single-vision correction) by 40% to 60% in children, on average,” Prof. Wolffsohn said. “Natural eye growth still occurs, but the child should end up less shortsighted than they would have been and their risk of visually impacting complications later in life reduced.”
An added bonus? “Our survey shows that practitioners’ job satisfaction goes up when they practice myopia control, and it is financially viable for their business,” Prof. Wolffsohn added.
Challenges in adopting certain myopia control strategies
Despite the availability of effective strategies, there are various reasons why some practitioners have been hesitant to adopt them universally. Concerns related to patient compliance, cost, and long- term efficacy have been cited as barriers to implementation. Additionally, limited training and access to specialized equipment or technologies necessary for certain interventions may also hinder widespread adoption.
“If practitioners don’t have the time or resources to do myopia management in their practice, they should co- manage with another optometrist or an ophthalmologist who does myopia management,” Dr. Kramer advised. “The more people understand how important this is, the more of a difference we can make.”
Navigating co- management challenges and opportunities
Apart from the co-management practices, awareness, and adoption of myopia management strategies, it is worth mentioning a few other critical issues related to myopia crossover between optometry and ophthalmology
Early Detection and Screening
Timely detection of myopia is crucial for implementing initiative-taking interventions. Optometrists and ophthalmologists could collaborate to establish standardized screening protocols, especially for high-risk populations such as children with a family history of myopia or those exposed to prolonged near work.
Patient Education
Educating patients and their families about myopia, its progression, and the available management options is vital. Practitioners can develop educational materials and counseling strategies to empower patients to take an active role in managing myopia.
“We’re more focused on the education part rather than the implementation, at least in the first visit,” Dr. Kramer said. “Especially if it’s a child’s first eye exam, those are some of the most challenging because not only do you have to diagnose them, but you also must explain that this condition is progressing and that now we need to do another treatment. It can be an overwhelming conversation. There’s a lot of new information, and sometimes you have to bring parents back for that,” she shared.
“We have a lot of educational materials. We give them resources where they can take the time to discuss these things with a partner or spouse or significant other, and then come back and make a decision,” she added.
Research and Innovation
Continued research and innovation are essential for advancing the field of myopia management. Optometrists and ophthalmologists can collaborate on research projects, clinical trials, and the development of innovative technologies or treatment modalities to further improve patient outcomes.
“Myopia control treatments are relatively new, so while the rate of them being prescribed is increasing, there is still a long way to go for a substantial adoption and practice will always lag attitudes,” Prof. Wolffsohn added.
Advancing myopia management for a clearer future
The crossover between optometry and ophthalmology in the management of myopia is vital for improving patient outcomes in an era of increasing myopia prevalence. By embracing a collaborative approach, optometrists and ophthalmologists can work together to enhance their understanding of myopia, adopt effective management strategies, and provide the best possible care for their patients. It is through interdisciplinary collaboration, research, and education that we can tackle the global challenge of myopia and ensure a clearer future for patients.
References
1. Holden BA, Fricke TR, Wilson DA, et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-1042.
2. Wolffsohn JS, Whayeb Y, Logan NS, et al. IMI – Global Trends in Myopia Management Attitudes and Strategies in Clinical Practice – 2022 Update. Invest Ophthalmol Vis Sci. 2023;64(6):6.
Editor’s Note: This article was published in COOKIE magazine Issue 12.